If you’ve ever heard of adenoididat all, it was probably in the context of a child having them removed. For something that plays such a crucial role in our early lives, adenoids remain one of the most misunderstood and mysterious parts of our anatomy. They’re like backstage crew in the theater of your immune system—you only notice them when something goes wrong.
So, let’s pull back the curtain. This isn’t just a medical explainer; it’s the story of a small piece of tissue that has an outsized impact on our health, especially when we’re young. We’ll explore what they are, what they do, why they sometimes cause trouble, and what happens when they’ve finished their job.
What Exactly Are Adenoids, Anyway? Finding the Unfindable
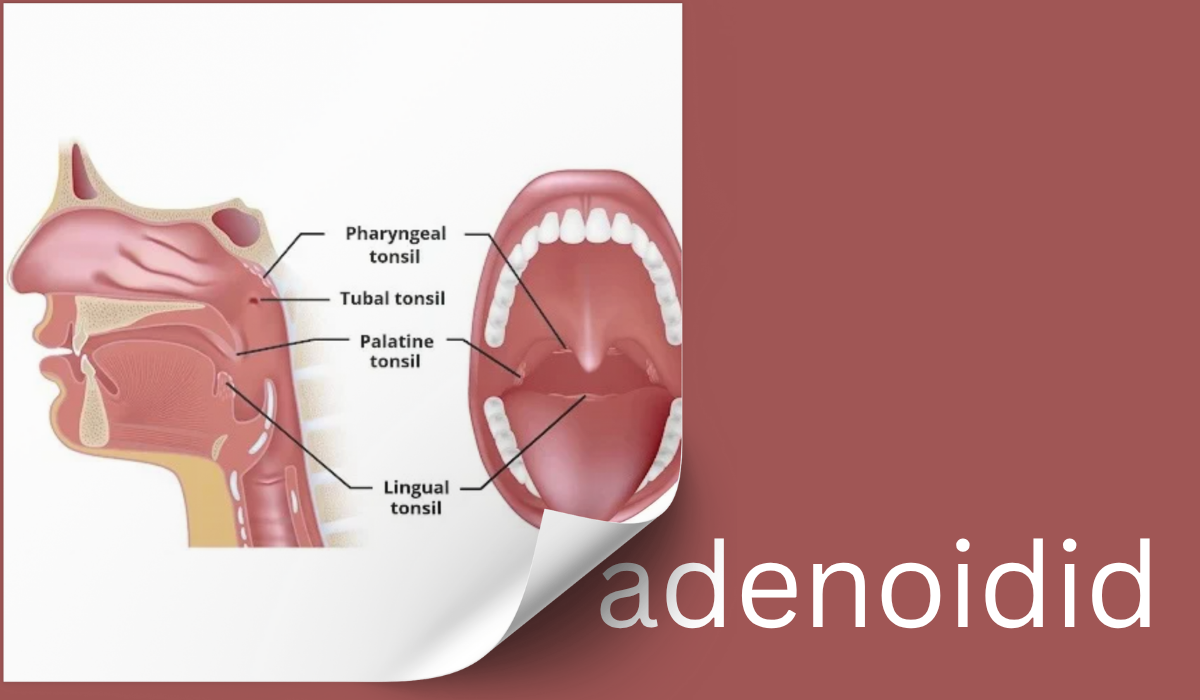
First, a crucial point: you can’t see your adenoids. Go ahead, stand in front of a mirror, open your mouth wide, and say “Ahhh.” You might see your tonsils dangling at the back of your throat, but your adenoids remain hidden. They live in the space where your nose meets your throat, an area called the nasopharynx. Think of them as cousins to the tonsils, made of the same lymph tissue, but stationed further up and behind your soft palate.
This location is strategic. They are positioned to be first responders, sampling every bit of air you breathe in and every germ that tries to enter through your nose. They are part of Waldeyer’s ring, a circular band of lymphoid tissue that acts as a security perimeter at the gateway to your respiratory and digestive systems.
In children, adenoids are relatively large, and this is by design. They are most active between the ages of 2 and 6, a time when kids are building their immune libraries, encountering countless new viruses and bacteria for the first time. The adenoids “train” the immune system by capturing these pathogens and presenting them to the immune cells, which then learn to produce antibodies to fight them off. It’s a busy, hands-on training ground.
The Trouble with Being a First Responder: When Adenoids Become a Problem
Here’s the catch. This very important job comes with a significant downside. Because they are constantly fighting germs, adenoids can become chronically infected or inflamed. This condition is known as adenoiditis (pronounced ad-uh-noid-EYE-tis).
Furthermore, simply being active immune tissue, they can grow too large, a condition called adenoid hypertrophy. Imagine a sponge that slowly expands as it soaks up water. Now, picture that sponge in a very cramped space at the back of your nasal passage. You can probably guess what happens next.
When adenoids become enlarged or chronically inflamed, they stop being helpful guardians and start causing a cascade of problems. The symptoms aren’t always obvious, especially in young children who can’t easily describe what’s wrong. Parents and doctors often have to play detective, looking for a constellation of clues.
The Tell-Tale Signs of Troublesome Adenoids:
- The Mouth-Breather: This is the most classic sign. A child with enlarged adenoids can’t breathe comfortably through their nose because the airway is physically blocked. You’ll see them with a perpetually open mouth, especially during the day when they’re focused on play, and at night while they sleep.
- The Noisy Sleeper: This goes beyond gentle snoring. We’re talking about loud, rattling, “can-hear-them-through-the-wall” snoring. But there’s more. You might also hear gasps, snorts, or even brief pauses in breathing—a sign of obstructive sleep apnea. This is a serious concern, as it disrupts the deep, restorative sleep crucial for a child’s growth and brain development.
- The “Glue Ear” Connection: The Eustachian tube, which connects the middle ear to the back of the throat, has an opening right next to the adenoids. When the adenoids get big, they can squash the opening of this tube, preventing it from draining fluid properly. This leads to a chronic, sticky fluid buildup in the middle ear, a condition called Otitis Media with Effusion (OME), or “glue ear.” The result? Muffled hearing, as if the world’s volume has been turned down, which can lead to speech delays and learning problems.
- The Nasal Voice and the “Adenoid Facies”: Because the nasal passage is blocked, the voice often sounds hyponasal—like they’re talking with a constant stuffy nose. Over time, chronic mouth-breathing can even alter facial development, leading to what doctors call “adenoid facies”: a long, narrow face, a high arched palate, and dental problems.
- A Persistent Runny Nose and Sinus Issues: Blocked drainage from the nose can lead to a constantly runny nose (often with clear mucus) and recurring sinus infections.
The Decision: To Remove or Not to Remove?
The term for adenoid removal is an adenoidectomy. It’s one of the most common childhood surgeries, but it’s never a decision taken lightly. Doctors don’t remove adenoids just because they’re large; they remove them when they are causing significant, documented problems.
So, how do you know if it’s time? The diagnosis isn’t based on a single symptom but on a pattern. An Ear, Nose, and Throat (ENT) specialist will piece together the story.
They’ll start with a thorough history, asking about sleep, breathing, and ear infections. Then, they might use a few tools to get a look at the elusive adenoids:
- A Flexible Nasal Endoscope: This is a thin, flexible tube with a light and camera on the end. The doctor gently guides it through the nose to get a direct, real-time view of the adenoids. It’s quick and provides the most accurate picture.
- A Lateral Neck X-ray: This simple X-ray can show the shadow of enlarged adenoids and how much they are impinging on the airway.
The “Green Lights” for surgery usually include:
- Moderate to Severe Sleep Apnea: This is a top reason, given the impact on a child’s health and development.
- Recurrent Ear Infections or Persistent “Glue Ear”: If fluid in the middle ear isn’t clearing and is affecting hearing, removing the adenoids can help the Eustachian tubes function properly. This is often done alongside the placement of ear tubes.
- Chronic Sinus or Nasal Infections: When multiple rounds of antibiotics fail to clear up chronic adenoiditis or sinusitis.
- Significant Impact on Quality of Life: When mouth-breathing and sleep disruption are affecting a child’s daily functioning, school performance, or dental health.
Life on the Other Side: The Adenoidectomy Experience
If surgery is recommended, it’s natural for parents to feel anxious. But understanding the process can help immensely.
The procedure itself is done under general anesthesia and typically takes less than 30 minutes. The surgeon removes the adenoid tissue through the mouth, so there are no external cuts or scars. It’s usually an outpatient surgery, meaning your child can go home the same day.
Recovery is generally straightforward but requires some patience. For about 7-14 days, there will be a sore throat, much like a bad case of strep throat. Bad breath is also completely normal and expected as the surgical site heals and scabs over. Soft, cool foods like ice cream, pudding, and mashed potatoes are your best friends during this time. The most important thing is to keep the child hydrated.
The results, however, can be dramatic. Parents often report a “night and day” difference. The child who was a restless, noisy sleeper suddenly sleeps peacefully and quietly. The chronic mouth-breather starts using their nose. The child who seemed to be in their own world, due to muffled hearing, becomes more engaged and responsive.
The Curious Case of the Disappearing Adenoid
Here’s the most fascinating part of the adenoid story: they largely retire on their own. As a child grows, their facial skeleton expands, making more room in the nasopharynx. At the same time, the immune system matures, and the body relies less on the adenoids for first-line defense.
By the late teenage years, adenoids have usually significantly shrunk (atrophied). In most adults, they have virtually disappeared. This is why adenoid issues are exceedingly rare in adults. They’ve served their purpose and gracefully bowed out.
You May Also Like: MyZaxbysFeedback Survey Rules, Rewards, and Entry Details
A Final Thought: Respect for the Little Lumps
Adenoids are a perfect example of a biological trade-off. For a period of our lives, they are essential, hardworking defenders. But their very function makes them prone to becoming a liability. They aren’t “bad” or “unnecessary”; they are a part of us that evolved for a specific phase of life.
The next time you hear about a child getting their adenoids out, you’ll understand the full story. It’s not the removal of a defective part, but rather a strategic retirement of a guardian that has, perhaps, become a little too overzealous in its duties. It’s a medical intervention that honors the fact that this small, unseen piece of tissue has a big job to do, and sometimes, needs a little help knowing when its work is done.